Glucosamine is a product that is almost a top-notch with degenerative inflammation in the market. There are many related health foods of various glucosamine, from glucosamine liquids, glucosamine ingredients to rubbed glucosamine. According to the l...

Glucosamine is a product that is almost a top-notch with degenerative inflammation in the market. There are many related health foods of various glucosamine, from glucosamine liquids, glucosamine ingredients to rubbed glucosamine. According to the long-term magazine report, the product value of health products related to "bone-related" in Taiwan is as high as 4.2 billion yuan. Yellow and coconut oil are both red goods for domestic health foods, but what effect does glucosamine have on treating or relieving degenerative inflammation? In medicine, we have a point-of-mouth. Today, let the nutritionists and doctors of the MedPartner team reply to the article to tell you, how much you can believe in this type of product!
What is glucosamine? What is the relationship with degenerative inflammation?Degenerative joint inflammation is a disease caused by the degeneration of the joints between the thigh and the calf and the knee. The obesity rate in modern people increases and lives longer. The incidence rate of this type of disease caused by pressure wear and degeneration is naturally increasing. Through medical imaging examination, it can be found that the soft bone wear and shrinkage of the joint cavity will cause pain and stiffness in clinical practice, and severe joints may deform. If you want to improve this situation, reduce the wear and tear of the joints, increase the hyperplasia of the joints, or increase the slippage of the joints fluid, are all feasible directions. If the hyaluronic acid injection in the cavity has been worn out, it is a common treatment method for surgical replacement of artificial hyaluronic acid, and there are also treatment methods for intravenous injection of hyaluronic acid in the cavity to increase slippage. Because glucosamine is one of the ingredients that form cortical bones and can be synthesized by the human body, it was considered to have the potential to improve degenerative cortical inflammation since decades ago, and a series of products and related research have also emerged like spring after rain.
glucosamine (2-amino-2-deoxy-D-glucose) is an aminomonosaccharide from chitin, which can be found in the exoskeletons of some marine invertebrates. This may not be a concept for everyone. The shell is an exoskeleton of marine invertebrates. Most of the glucosamines that everyone eats are fermented from crab shells, mushrooms, or bacteria! In addition to shells or shells of crabs, glucosamine can be extracted from natural foods, some bacteria also contain glucosamine (Ref 17). However, when we usually eat crabs, we will not eat shells, and it is even more impossible for someone to eat shells without any trouble, nor will they eat bacteria in order to extract glucosamine. Therefore, it is actually not feasible to take glucosamine from natural foods. Since it is difficult to get from food, the next thing to know is the question of "whether to supplement additionally"!
glucosamine is a non-cellular component that is necessary in lint tissues, bones, and vegetation. It mainly includes three types (Ref 1):
●glucosamine sulfate (glucosamine sulfate)
●glucosamine hydrochloride (glucosamine hydrochloride)
●N-acetylglucosamine (N-acetylglucosamine).
In all relevant studies of glucosamine so far, glucosamine in the form of "salt sulfate" is more likely to be effective. Currently, the domestic salt sulfate type of glucosamine is considered to be a doctor or a physician for instructions for drug management (no prescription label required). There is only an oral agent to relieve the pain of degenerative inflammation, but it has not been made into a topical agent. Other forms of glucosamine are currently considered "food" to be managed, which means that in addition to glucosamine sulfate, whether eaten or wiped, the government's position only needs to be safe and does not need to prove that it is effective, but it cannot be claimed to be effective in the law.
Although the regulations cannot declare effective, are these products effective? Let’s take a look at what the relevant research results are said! The following is a compilation of research for medical references. It may be a bit difficult for everyone to read. You can see the key points you should know by reading them in rough words!
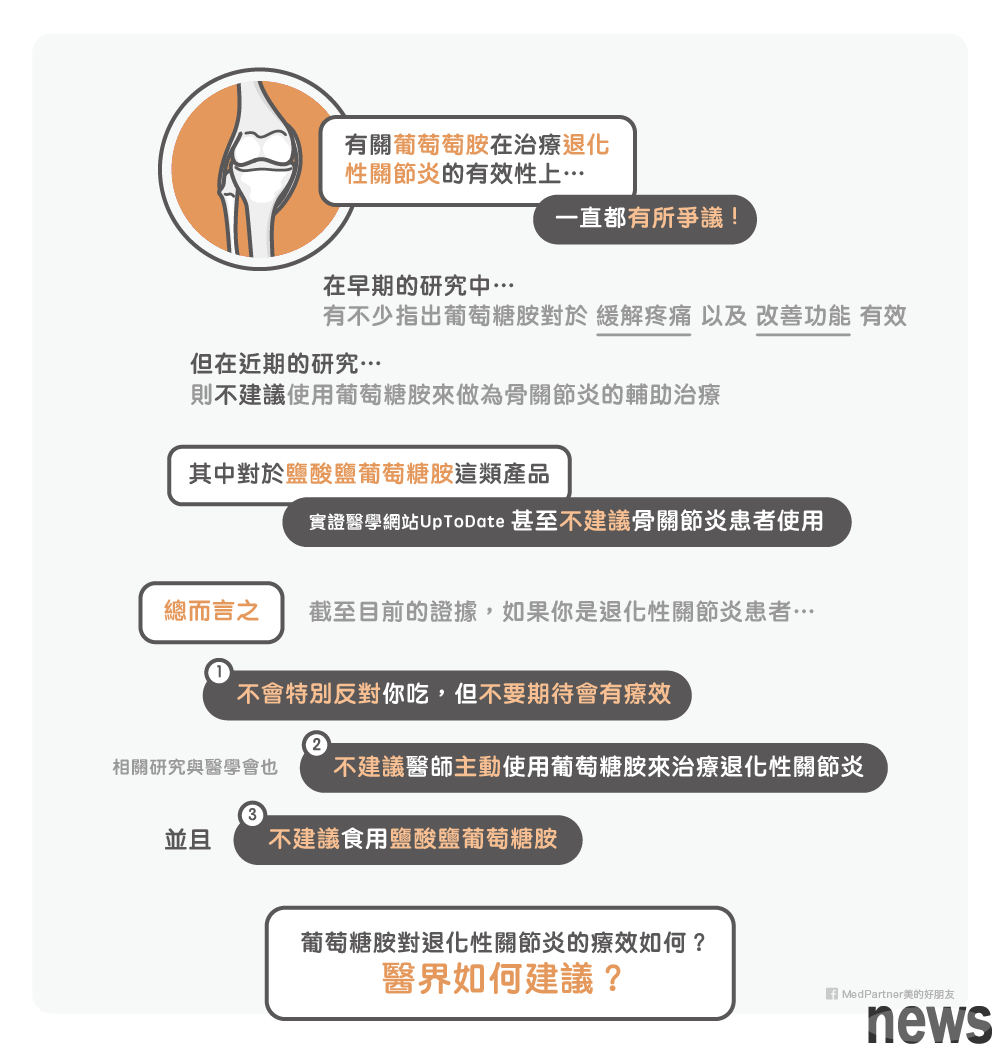
How effective is glucosamine in the treatment of degenerative inflammation? How did the medical community suggest?There has been a constant debate on the effectiveness of grape amine in the treatment of degenerative inflammation. In early studies, many pointed out that glucosamine is effective in relieving pain and improving function. However, in recent studies, results that were inconsistent with earlier studies have emerged. Related treatment guidelines from 2008 to 2013 do not recommend glucosamine as a supplementary treatment of osteopathic inflammation.
After singularly revisiting the article, products such as salt glucosamine found that they have no improvement effect on pain, and the actual medical website UpToDate even directly does not recommend patients with osteoarthritis to use salt glucosamine.
That is to say, according to the current evidence, if you are a patient with degenerative inflammation, you will not specifically object to taking glucosamine products, but do not expect it to be effective. Moreover, these related studies and the medical community do not recommend that doctors actively use glucosamine to treat degenerative inflammation. If you eat salt glucosamine, please save it, it won't be good for you.
The following are related research and collections for professionals to refer to:
Is it recommended to use glucosamine in patients with inflammatory diseases?The use of glucosamine is still controversial, with opinions on both sides.
Suggestions:
●The European Union for Preventing Wet Diseases’ Recommendations for Hand Osteopathy in 2007: This article reviewed 15 random control experiments, and 14 of the 15 articles used salt glucosamine sulfate, 1 used salt glucosamine sulfate, 12 used osteopathy for angular cervical osteopathy, 2 for angular symmetry and gangular symmetry, and 1 for 1 without special targets for specific parts. The results show that glucosamine withdrawal is effective for patients with osteoarthritis, but is ineffective for improving physiological function or physiological stiffness (Ref 7).
●The European Union for Prevention of Wet Diseases proposed in 2005 for facial osteoarthritis: As of 2007, there were studies on glucosamine, but there were few cases of facial osteoarthritis. In the study of combined joint and knee joint inflammation, glucosamine intervention is significant for improving pain and function. (Ref 8 )
●The European Union for Preventing Wet Diseases proposed in 2003 on angular osteoarthritis: Similar to the two guidelines mentioned above, the researchers conducted a statistical analysis of many glucosamine and angular osteoarthritis, and pointed out that glucosamine is effective in improving pain, but depends on the severity of the pain disease. Glucosamine intervention in moderate to severe patients is ineffective (Ref 9 ).
●International Osteopathic Inflammation Research Association proposed a guide for the 2007 symmetry and knee osteopathic inflammation: This guide mentioned that after 20 randomly compared experiments, it was found that if the Lequesne scale was used as an evaluation tool, it was shown that glucosamine can improve knee pain by 28% and 21% improvement in function; but if the WOMAC scale is used, there is no improvement in pain and function (Ref 10).
Not recommended to use:
●American Society for Wet Diseases Non-pharmacological and pharmacological recommendations for osteopathic inflammation (Ref 3).
●Plastic Surgery of the American Physical Treatment Association In 2009, the Guidelines stated that the results of various glucosamine-related studies as of 2009 were inconsistent, and the studies that showed that effective were short-term improvements in pain or function rather than long-term, so use was not recommended (Ref 4).
●The American Orthopedic Medical Association's 2013 Guidelines for Treatment of Osteopathic Inflammation: This guideline combines 12 studies on glucosamine and dermatitis for statistical analysis, and believes that glucosamine has no significant effect on improving dermatitis (Ref 5).
●The Royal College of Medicine's Guide for Adult Osteopathic Inflammation in 2008: This guideline mentioned that salt glucosamine sulfate seems to have a pain-reducing effect on osteopathic inflammation, but at that time, because the UK did not have permission to use glucosamine sulfate, it was not recommended to use this guideline. The salt glucosamine, which could be used in the UK at that time, was unable to achieve significant effects in many studies (Ref 6).
If we look at the above guidelines in detail, it is not difficult to find that the first three guidelines for the use of glucosamine all come from the same organization, and it is recommended that the guidance for glucosamine can be used is more than ten years away. The glucosamine ten years ago seemed to be a great blessing for patients with osteoclastitis. When looking for literature, the author also found that glucosamine-related research, which has been more and more, seems to be effective in improving the symptoms of osteoclastitis, but with the advancement of the times, more and more research has been made, and the results do not seem to be so significant. Therefore, 2008 to 2013 No annual guidelines recommend the use of glucosamine as aid in the treatment of osteopathic inflammation.
It is worth mentioning that as early as ten years ago, there was a review article exploring why the results of the research on glucosamine and osteopathic inflammation are always inconsistent. In this paper, China Overseas selected 128 studies on glucosamine, excluding studies with poorly designed research, and finally 15 double-blind randomly compared with experimental research for statistical analysis. It was found that if salt glucosamine is used as the supply form, there will be no improvement effect on pain. The same opinion as the review in this article is the website of the verified medical treatment. UpToDate, they directly do not recommend that patients with osteoarthritis use salt glucosamine acid; while the research results are very different with salt glucosamine sulfate as the supply form. The authors believe that this is because most of the studies have been involved in manufacturers, so it cannot be used as a good reference indicator (Ref 11).
Newer study●A double blind random group experiment published in 2015 was divided into four groups with 605 middle-aged and elderly people with chronic knee pain and narrow femur of love bones and femur. The first group was a control group for evacuating comfort agents, the second group to the fourth group was a evacuating 1500 mg of salt glucosamine sulfate and evacuating 800 The experiment group of mg of salt sulfate, glucosamine sulfate plus salt sulfate and sulphate sulfate was followed for two years, and knee pain symptoms and physiological functions were evaluated using the WOMAC scale, and the knee space narrowing was measured by X-ray. The evaluation was conducted separately before, one year after the intervention, and two years after the intervention. Finally, 502 subjects completed the experiment completely. It was found that after two years of intervention, the narrowness of the correlation space in the glucosamine and solutein group showed a significant decrease of 0.1mm than that of the control group, and there was no significant difference in the narrowness of the correlation space in the other groups after one year of intervention or two years; and in the part of knee pain or physiological function, there was no significant difference between the groups, regardless of one year of intervention or two years (Ref 2).
●A double blind random group experiment published in 2014 was a total of six months of trials. The patient was divided into two groups, one was taken from 200 mg of NSAID drug celecoxib, and one was taken from 1500 mg of salt glucosamine salt acid plus 1200 mg of salt sulfate solutin sulfate. The intervention time was six months in total. The final part of the trial was 240 and 225. It was found that the WOMAC pain scores were reduced by 185.7 and 186.8 respectively, and there was no significant difference between the two groups; among the subjects who completed the OMERACT-OARSI standard, the correlation dysfunction of the two groups decreased by more than 50%, and there was no difference between the other results. Therefore, this study believes that the treatment of combining glucosamine and solulin is as effective as NSAID drugs (Ref 16).
Recent studies seem to be focusing on the combination of glucosamine and somatosinolates. From the above two studies, it seems that the combination of the treatment of the two is partially beneficial for osteopathic inflammation. However, it is worth noting that the second study design does not contain a control group for soothing agents, so further research still needs to prove the effect.
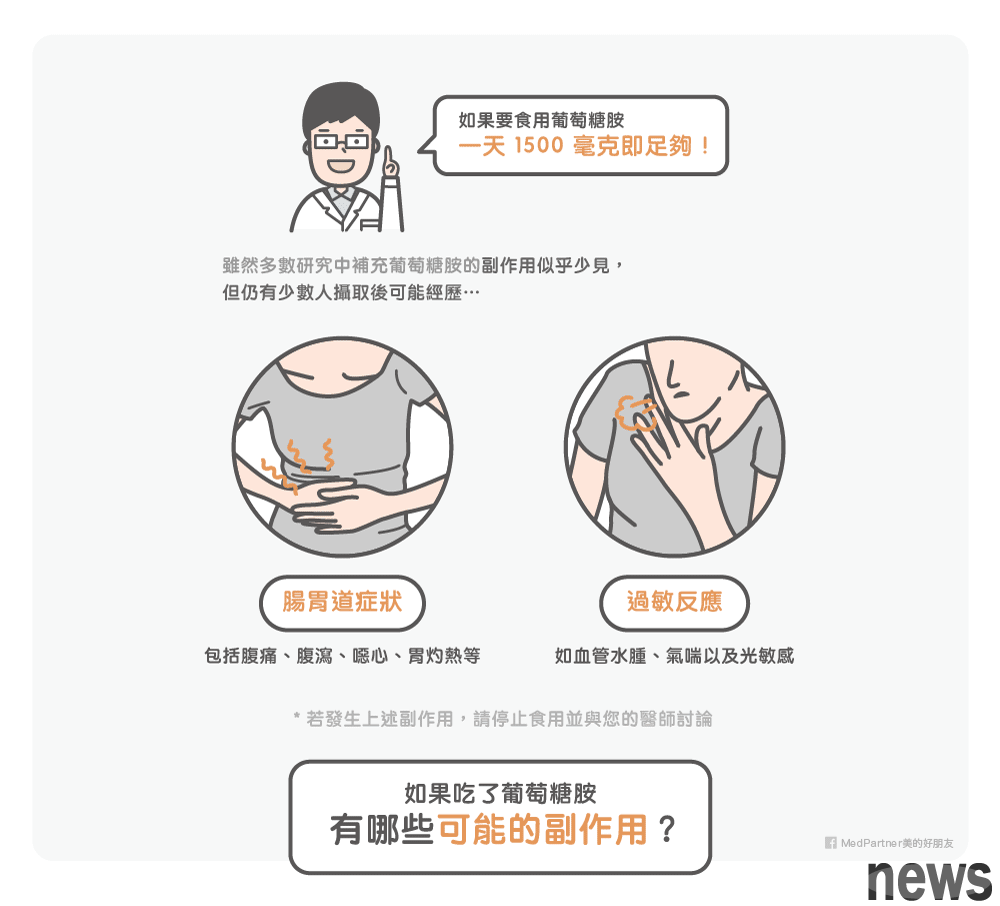
If glucosamine is to be taken, how much dose is it safe to take? What are the possible side effects?If you want to take glucosamine sulfate, doctors and pharmacists will not specifically encourage you, but they will not particularly impede you. And salty glucosamine is really not needed. But how much should I eat? After the examination, taking 1500 mg of glucosamine is enough, and the concentration in the bleeding will continue to increase intentionally. Although the side effects of glucosamine supplementation appear to be rare in most studies, a small number of people still have gastrointestinal symptoms after intake, including abdominal pain, abdominal pain, nausea, heartburn, etc., and a few people have allergic reactions such as vascular hydration, asthma, and light sensitivity (Ref 1).
The following studies are compiled for professional reference:
Although glucosamine was used for various studies a long time ago, it was not until 2005 that the first drug dynamics experiment with humans was found. In this study, 12 healthy people were randomly divided into subjects, taking 750, 1500, and 3000 mg of glucosamine each day, and was given in one go. It was found that glucosamine drug dynamics showed a linear relationship when the dose was 750 and 1500 mg, but not at 3000 mg. After about 3-4 hours of oral administration, the glucosamine concentration in the blood hydrate rose to the highest value, indicating that the bioavailability of glucosamine was not low, and then slowly decreased to almost return to the base value at 48 hours. The original blood glucosamine concentration of these 12 healthy subjects fell between 10.4 and 204.0 ng/ml (equivalent to 0.06 and 1.1 uM), and the highest blood concentration after 1500 mg of glucosamine was about 10uM, which the researchers defined as 30 times the base value. The exclusion half-life of glucosamine is approximately 15 hours. Many related studies of glucosamine use 1500 mg as the intervention dose, and the results of this study also support that 1500 mg seems to be the appropriate dose (Ref 12).
Another glucosamine comparison is often discussed about its related effects on glycoprotection and insulin sensitivity. There are two main theories that may be this doubt. The first is glucosamine, which is one of the suprasing products of glucose, so some say that it may be the source of glucose, but because the enzymes in the pathway of glucose in the human body are irreversible, this theory does not hold true; the second is that oral glucosamine is taken to affect the original hexacosamine synthesis pathway and interfere with endogenous glucosamine, and hexacosamine synthesis pathways are generally considered to play an important role in human blood glucose condition (Ref 13).
●A random double-blind controlled study consisted of 54 patients with type 2 diabetes, divided into control groups for placement and a 1500 mg salt glucosamine salt acid for 12 weeks, and fasting blood glucose, insulin were measured at 0, 8 and 12 weeks, and HOMA-IR and QUICKI were measured at 0, 8 and 12 weeks. Assessing insulin sensitivity, it was found that at each time, there was no significant difference between the groups. Therefore, this study concluded that continuous 12-week glucosamine intake will not have adverse effects on blood sugar control and insulin resistance in patients with type 2 diabetes (Ref 13)
●Another random double-blind control study, 38 patients with type 2 diabetes were given as subjects, divided into control groups for placement injections and 1500 mg of salty glucosamine with salty acid plus 1200 The experimental group of mg of salt sulfate solutein sulfate was 90 days of intervention and used glycated hemoglobin as a glycogenic indicator. It was found that there was no significant difference in the two groups of glycated hemoglobin after 90 days of intervention. Therefore, the conclusion under the authors is that glucosamine will not affect the blood glucose enhancement of diabetic patients during the 90-day intervention (Ref 14).
●A study published only at the end of 2016, in which 407 middle-aged women with BMI>27 were taken as subjects, allowing patients to take placement agents or oral glucosamine sulfate to follow up for 6.5 years, and after 1 year, 2.5 years, 6.5 years. A questionnaire was conducted annually and a questionnaire survey was conducted. It was found that the long-term glucosamine-induced glucosamine was compared with the control group, and the incidence of glycated hemoglobin or diabetes was slightly increased, but there was no significant difference (Ref 15).
Although the above two studies on diabetes patients as the subjects both pointed out that glucosamine does not affect the blood sugar of diabetic patients, since the intervention time is only three months, whether it will affect blood sugar if longer-term use is still unknown. Therefore, it is recommended that if diabetic patients want to take glucosamine, they should still discuss it with the doctor and inform the doctor.. Many other studies that have considered healthy people without diabetes as subjects have also shown that glucosamine does not appear to affect blood sugar or insulin resistance.
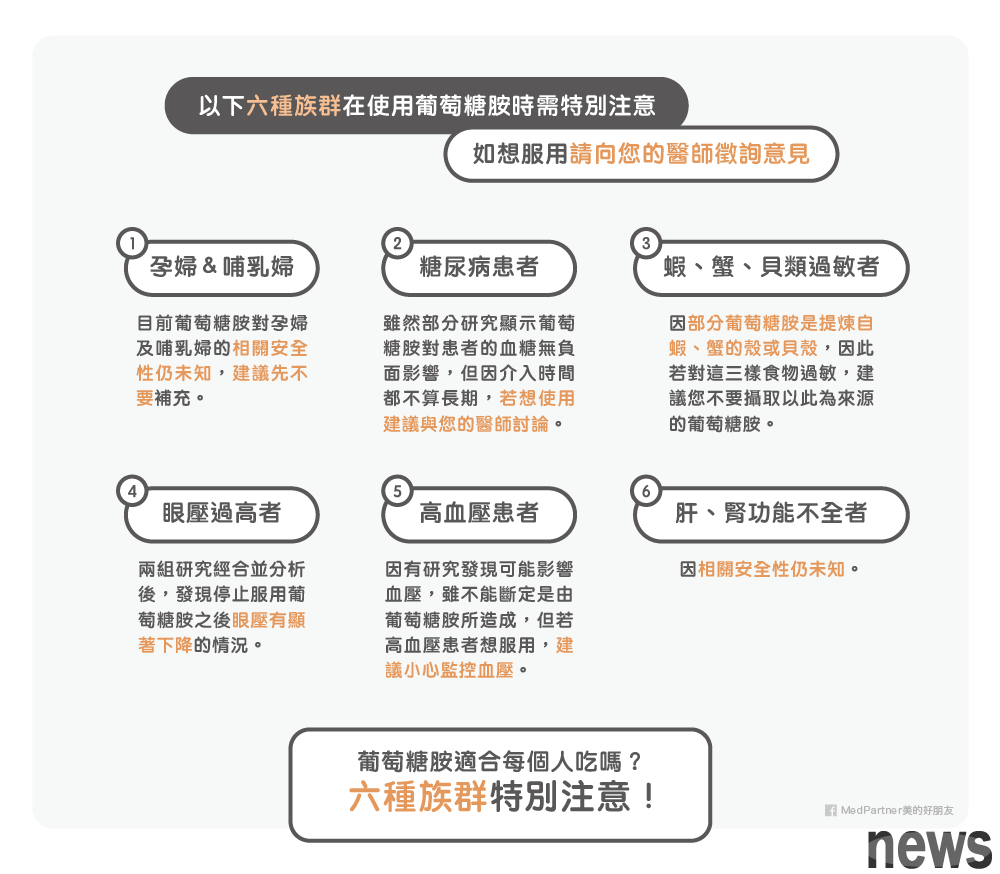
Is glucosamine suitable for everyone to eat? Please pay attention to the following 6 kinds of people!Glucosamine is like all health foods. If you want to use them, you must "firstly talk about whether you will not harm your body, and then try to find out the effect." Here are six groups that need special attention when using glucosamine. If you really want to take it, please contact your doctor for advice!
1. Pregnant and breastfeeding women: At present, the relevant safety of glucosamine for pregnant women and breastfeeding women is still unknown, so it is recommended that pregnant and breastfeeding women not replenish them first.
2. Diabetic patients: We have discussed the relationship between glucosamine and blood sugar (Ref 13, 14, 15). Although some studies have shown that glucosamine will not have a negative impact on the blood sugar of diabetic patients, however, because the intervention time is not long-term, if you are a diabetic and want to use glucosamine, it is recommended to discuss with your doctor.
3. Allergies with sap, crab, and beans: Because some glucosamine is a shell or bean that increases self-causing, crab, or beans, if you are allergic to these three foods, it is recommended not to take glucosamine from this source.
4. Over-empty person: A study divided 17 subjects into two groups, and 11 subjects in Group A measured eye pressure before starting glucosamine; 6 subjects in Group B did not measured eye pressure before taking glucosamine. Each patient in the two sets took different amounts of glucosamine, but most patients took 1500 mg per day. It was found that the eye pressure of the subjects in Group A showed a significant increase in their eye pressure after starting to take glucosamine, and the eye pressure decreased significantly after stopping taking glucosamine; patients in Group B showed a significant decrease in their eye pressure after stopping taking glucosamine. If the two groups were combined for statistical analysis, it was also found that the eye pressure decreased significantly after stopping taking glucosamine (Ref 18).
5. Patients with hypertension: In a study, it was found that six weeks after the subjects were taken with nutritional supplements containing glucosamine, the patient's suppleness pressure decreased significantly, the contraction pressure was a tendency to decrease, and the heartbeat rate also increased. The supplement used in this article also contains other ingredients such as solutein and collagen (Ref 19), so it cannot be determined that this result must be caused by glucosamine. If patients with hypertension want to take glucosamine replenishment, it is recommended to monitor blood pressure carefully.
6. People with liver and kidney insufficiency: due to unknown safety.
In addition, there is one thing to note when taking glucosamine. Most of these products contain salt or calculator. People with special diseases that are restricted by the load or calculator can pay attention to the mark when taking it and carefully calculate the calculator content. Generally, normal people recommend that the daily loading capacity is less than 2400mg, so be careful!
After reading this long article, I believe everyone has a correct and complete understanding of glucosamine! If you suffer from degenerative symptomitis, please seek a complete evaluation and treatment for the doctor. Health food is at most a helper role under the instructions of the doctor! It is an unrealistic fantasy to use health foods to cure degenerative inflammation! The market and interests of health food industry are amazing, and the information found online is difficult to avoid business influence. I hope that the compilation of this article will help more people and evaluate whether you need to use glucosamine under a clearer understanding of your situation.